Herpes Zoster (HZ)
Herpes Zoster (HZ), also known as shingles, is a common and debilitating disease caused by the reactivation of the Varicella Zoster virus (VZV), a DNA virus belonging to the Herpesiviridae family, generally contracted during childhood.
Following a primary infection, which manifests as varicella (chicken pox), the virus becomes latent in the cranial and spinal cord sensory ganglia, and can be reactivated giving rise to nerve and skin manifestations with a dermatomal distribution typical of HZ. The incidence rises with increasing age and/or reduction of the cell-mediated immune response.
Memory T cells specific for Varicella Zoster virus, in fact, reduce with age; this decline becomes significant after the age of 50 and correlates with an increased risk of HZ. About 90% of patients with HZ are immunocompetent. Herpes Zoster, unlike chickenpox, does not have a seasonal or epidemic pattern in its spread. Several studies suggest that in addition to age, medical conditions such as diabetes, major depression, stressful life events, or immunosuppressive treatments may increase the risk of HZ, as they can reduce the cell-mediated response to the virus.
Transmission routes
The transmission of Varicella Zoster virus from a person suffering from HZ to a susceptible healthy subject (who has not had chickenpox and who has not been vaccinated) can occur through direct contact with the skin lesions, as the virus is contained within them. The lesions initially appear as erythematous papules which then evolve into vesicles and subsequently into pustules that heal over a period of 7-10 days. The subject can be considered non-contagious when all of the lesions have healed. In the event of infection, the subject will develop Varicella and not HZ, as HZ is a late complication of varicellar infection. Moreover, unlike that which happens with Varicella, in the presence of HZ the virus does not spread via air: indeed, in this case, the virus does not affect the upper respiratory tract. A person with Varicella cannot transmit HZ, as this pathology is determined by a reactivation of the virus that has remained in a latent state in the cranial and spinal cord sensory ganglia. This reactivation can occur following a reduction of the cell-mediated immune response and not through new exposure to the virus.
Symptoms and complications
The most frequent site of HZ is on the thorax, with skin rash and neuralgia that are usually limited to a ‘band’ on one side of the body (hence the name "Zoster", which in Greek means "belt"). Initially the rash is erythematous with maculo-papular lesions which subsequently become vesicular. New lesions may continue to appear for up to 7 days, after which scabs form, disappearing in 2-3 weeks. The pain typically precedes the vesicular rash by 3-5 days and in some cases by several weeks (prodromal neuralgia). The form which affects the ophthalmic branch of the trigeminal nerve, often referred to as ophthalmic HZ, accounts for 10-20% of cases of HZ (more frequent with increasing age).
Almost half of these subsequently present ocular complications, such as neurotrophic keratitis. The most frequent complication of HZ is post-herpetic neuralgia: a neuropathic syndrome which occurs, or persists for, at least 3 months following the onset of rash or acute pain from HZ. It is characterised by pain along the cutaneous nerve endings that can manifest with one or more painful or paroxysmal attacks, burning or stabbing with a spontaneous onset, and linked to changes in sensitivity to various sensory and pain stimuli (defined as paresthesia, dysesthesia, allodynia and hyperalgesia ). In Italy a recent study, carried out through a network of general practitioners, showed that in, respectively, 20.6% and 9.2% of patients with HZ, post-herpetic neuralgia was present at 3 and 6 months, negatively affecting quality of life. The duration of pain associated with HZ increases with advancing age and is greater in subjects aged 70 or older.
The persistence of painful episodes with functional nerve alterations up to 10 years from the acute phenomenon has been documented. Possible non-neurological complications are also frequent, including bacterial superinfection of lesions, with scarring, cutaneous dissemination, pneumonia, myocarditis, esophagitis, pancreatitis, gastric ulceration and granulomatous angioitis.
Impact on the population
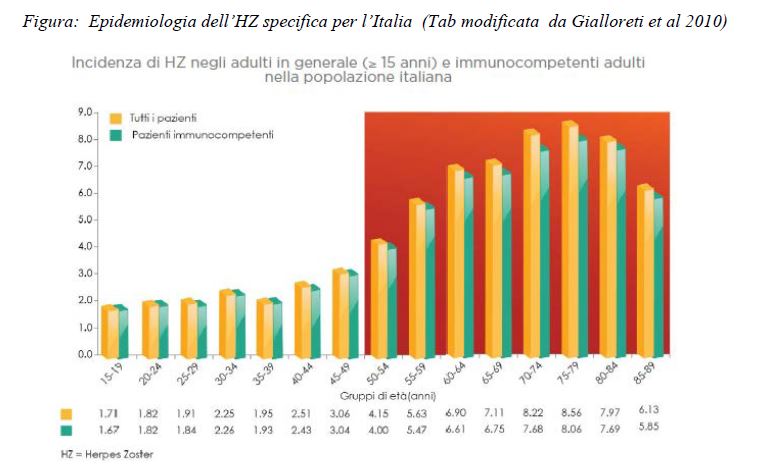
The incidence of HZ is similar throughout the world and correlates to the age of the population: from 2-3/1000 people a year between ages 20 and 50 to 5/1000 in the sixth decade of life and 6-7/1000 in the seventh to eighth decades, with a peak in subjects of 75-79 years of age. In the United States, Canada and Europe the estimated annual incidence is 3-4 cases per 1000 person-years. With the increase in the elderly and fragile population, a rise in HZ cases is expected in the near future. On average about one person in 4 develops HZ over the course of their lives and the disease affects about half of those who reach 85 years of age. In general, HZ occurs only once in an individual's life, however, it is possible that even immunocompetent individuals may suffer from multiple episodes of HZ with a recurrence rate ranging from 1.5 to 12.5%. In Italy, an estimated 157,000 new cases of HZ occur each year. In the 1999-2005 period, there were 35,328 hospitalisations, most involving subjects over the age of 65, with an average stay of 8 days and a total of over 22,000 inpatient days per year.
Clinical-therapeutic management of HZ is complex and often unsatisfactory. In the acute phase, the primary treatment is antiviral drugs which are used to relieve pain during this phase and to limit the spread and duration of dermatological lesions, as well as the frequency and severity of complications. They should be administered within 72 hours of the onset of the rash and treatment is generally continued for 7 days. Oral corticosteroids, NSAIDs, opioids, tricyclic antidepressants and anticonvulsants, are also used for acute pain management, with variable efficacy. The combined use of multiple drugs is curtailed by the risk of side effects, among other things. The effects of pain, especially if prolonged, significantly impede the quality of life and their management is often considerably complex. HZ vaccination is therefore a possible alternative solution to prevent the onset of the disease.

Ophthalmic Herpes Zoster with uveitis and keratitis

Characteristic rash of Herpes Zoster on the thorax