Vaccinating against Bacterial Meningitis
The epidemiological curves comparing pre- and post-vaccination periods show a sharp decrease in the number of cases over the years. It is clear that vaccinations have significantly changed the incidence of diseases for which immunisation exists, thus saving lives, reducing disease outcomes, reducing overall population suffering and improving quality of life.
The disease before and after the vaccination campaign in Italy
In Italy, a surveillance system dedicated to bacterial meningitis has been active since 1994 and has expanded since 2007 to include all invasive meningococcal, pneumococcal and haemophilic diseases. This surveillance, coordinated by the Istituto Superiore di Sanità (Italian Institute of Public Health), is carried out on a nationwide basis.
Haemophilus influenzae infection: Hib meningitis
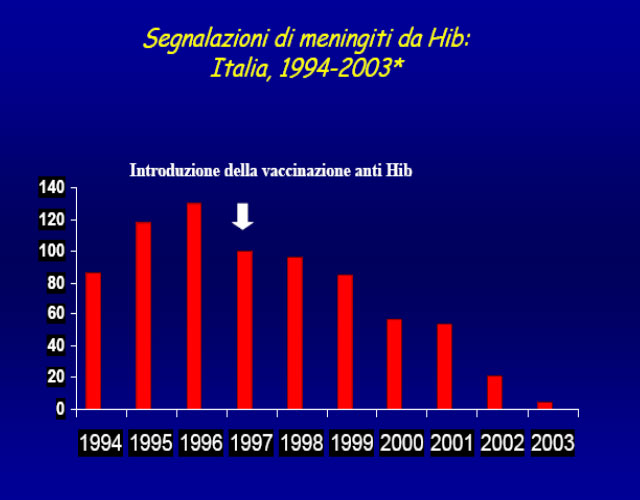
Hib vaccination was introduced in 1995 and added to the National Vaccination Schedule in 1999. Vaccination coverage reached 95.6% in children at 24 months of age (2009 data, DG Prevention – Italian Ministry of Labour, Health and Social Policy). As seen from the graph below, over the years, with the increase in vaccination coverage the incidence of invasive Hib infections decreased.
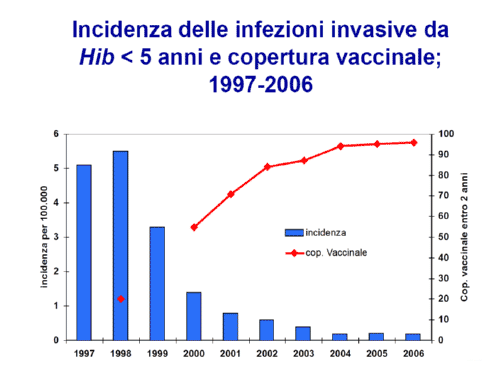
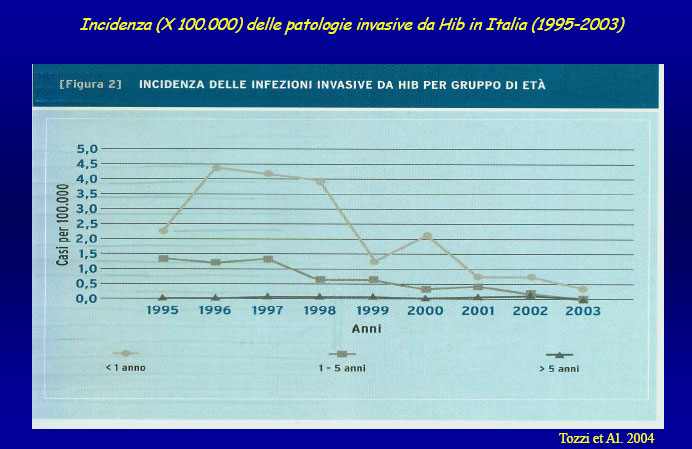
Thanks to a strong vaccination campaign, Haemophilus influenzae has gone from being the most frequent pathogen responsible for bacterial meningitis to one of the least frequent. However, it still requires constant attention. The infection can affect anybody and is the cause of meningitis and sepsis; described cases of vaccination failure are rare.
Meningitis caused by Neisseria meningitidis (meningococcus)
In Europe the meningococcal conjugate vaccine was introduced in 1999. In countries like the United Kingdom where vaccination campaigns for different age groups have been in force since the end of the nineties, cases of invasive meningococcal disease have decreased significantly, as the following graph shows:
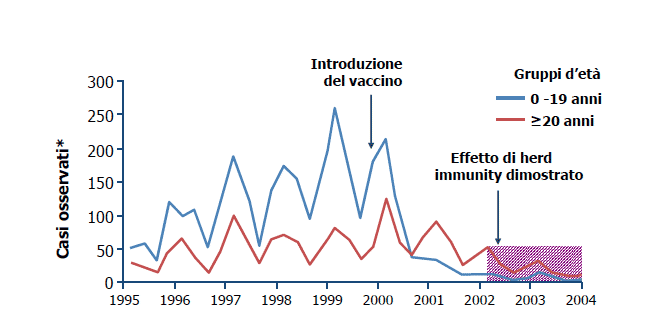
In Italy, the 2012-2014 National Vaccination Plan introduced the meningococcal conjugate vaccine for all newborns at the 13th month (single dose) and also for all those not previously vaccinated aged between 11 and 18. Previously, the vaccine had been recommended only for those at risk, and since 2006 Italian regions have begun to offer the vaccine, although with different terms of supply.
As can be seen from the table below, over the years the number of cases of invasive meningococcal C disease has decreased starting from 2005, the year that universal childhood vaccination was introduced in many Italian regions. The most affected groups remain 1- to 4-year-olds with a second peak in adolescents.
Nevertheless, the progression of invasive meningococcal disease confirms the need to continue vaccination in the first year of life and in adolescents.
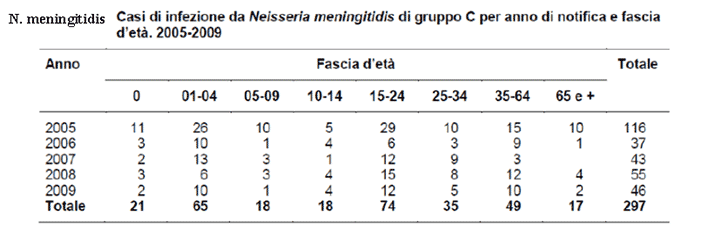
ISTISAN Report 12/25: The surveillance of meningitis and other invasive bacterial diseases in Italy, years 2005-2009
Invasive Disease caused by Streptococcus pneumoniae (pneumococcus)
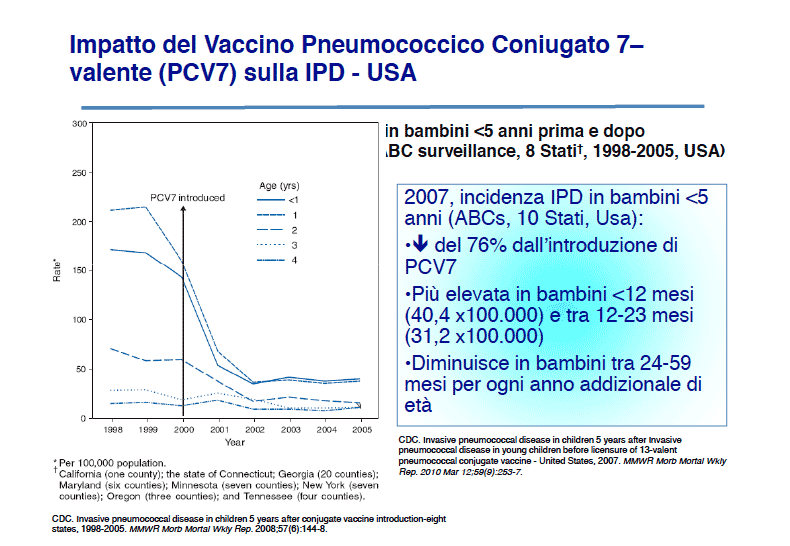
Invasive pneumococcal disease is a seasonal disease that can affect any age group, but is more frequent in children between 2 months and 3 years of age, with incidence peaks between 6 and 18 months, and in the elderly. Streptococcus pneumoniae can cause, in addition to meningitis, clinical pictures of sepsis (generally with a high fever, not as severe as meningococcal sepsis) pneumonia or infections of the upper respiratory tract, such as otitis. As can be seen from the graph below, the introduction of immunisation with the pneumococcal vaccine has significantly modified the epidemiology of the disease in the USA.