Vaccines do not cause autoimmune diseases
The hypothesis
Stimulating the immune system with vaccine antigens, or with adjuvants and other components of vaccines, can lead to the development of an autoimmune reaction and therefore to autoimmune diseases.
Three unfounded "immunological" criticisms of vaccines
At least three immunological criticisms are made against vaccines1.
The first is that the immunity induced by vaccines, compared to that arising from natural infection, is less robust and has a shorter duration. This criticism is laughable when one considers that the cost of immunity acquired through infection is the risk of developing the disease. The success of vaccinations, demonstrated by the disappearance or drastic reduction of vaccine-preventable diseases, is the best proof that the immunity induced by vaccination, perhaps in some cases lower than that induced by infection, is nonetheless more than sufficient1-3.
The second criticism is that the antigenic overload caused by vaccination can lead to damage or even to paralysis of the immune system. This criticism also stems from a lack of factual knowledge. Adding up all 15 vaccines that are administered, the alleged "antigenic load" is 130 protein or polysaccharide antigens for a total of 163g of antigen. As a comparison: the pertussis vaccine contains three antigens, while a single Bordetella pertussis has more than 2,000. Vaccines are therefore a drop in the ocean of the antigens that the child eats or breathes every day. The antigenic load is therefore an unfounded problem.
The third criticism is that vaccinations trigger immune mechanisms and therefore autoimmune diseases.
Scientific elements that disprove a causal relationship between vaccines and the development of autoimmunity and autoimmune diseases
The hypothesis of a role played by vaccinations in causing autoimmunity and autoimmune diseases is based exclusively on anecdotal cases or unverified observational studies describing the development of autoimmune mechanisms which are nonetheless fleeting and which never trigger autoimmune diseases . It is indeed well known that robust control mechanisms1-3 are present in the immunological system.
A biological plausibility to suggest a causal link between vaccines and autoimmune diseases could be proposed for Guillain-Barré syndrome and the swine flu vaccine or the oral polio vaccine, or for chronic arthritis or thrombocytopenia and the rubella vaccine . In other scenarios, such as measles vaccination and the development of type I diabetes, plausibility is merely theoretical5-7.
Strictly controlled and rigorously performed studies have ruled out plausibility. The Institute of Medicine has reviewed more than 12,000 reports, ruling out any relationship between vaccinations and type I diabetes or Guillain-Barré syndrome. Similarly, any relationship between multiple sclerosis and Calmet-Guérin bacillus and vaccines against typhoid, hepatitis B, influenza, and polio have been excluded8-11.
Molecular mimicry between epitopes of pancreatic and enterovirus cells, cytomegalovirus, rotavirus, rubella virus or mumps does not trigger the development of pancreatic autoimmunity and diabetes. Indeed, where universal vaccination against measles, mumps and rubella has been carried out, a decrease in the incidence of type I diabetes has been observed.
In two conditions a causal link between vaccination and development of autoimmunity has been demonstrated. The first consists of autoimmune thrombocytopenia and the MMR (measles, mumps and rubella) vaccine. Autoimmune thrombocytopenia appears in 1 in 30,000 vaccinated children, but it must be taken into consideration that autoimmune thrombocytopenia develops in 1 in 3,000 children with rubella and 1 in 6,000 children with measles1-4-6. Thus, even for these two conditions the balance is largely in favour of vaccination.
Adjuvants and preservatives
Adjuvants are products added to vaccine preparations in order to reduce the dose of vaccine antigen while maintaining the effectiveness of the vaccination. Squalene is a tripentene produced by all higher organisms including humans, and is present in numerous foods as well as in cosmetics. Squalene was suspected of playing a role in Gulf War Syndrome that affected American veterans of the first Gulf War. These veterans had anti-squalene antibodies in a high proportion and this was attributed to the squalene that was said to be present in the anthrax vaccine. However, a similar proportion of antibody-positive subjects was present in the control population. Furthermore, the anthrax vaccine did not contain squalene12-13.
In some animal models (with no human counterparts) massive doses of mercury can cause autoimmune vascular reactions. Mercury, in the form of ethylmercury, was present as a preservative in some vaccines. However, the quantity of mercury that was taken by children via vaccines was well below any safety threshold. Furthermore, the mercury that causes illness is not ethyl mercury, but methyl mercury, which is found in food and especially in fish. In any case, at present no vaccine contains mercury - a decision that was taken not because it causes damage, but rather to eliminate this specious excuse14.
In contrast, infections (which can be defeated by vaccines) trigger autoimmune mechanisms and autoimmune diseases
A great deal of scientific data, acquired using rigorous methodologies, unequivocally demonstrate that infections trigger autoimmune mechanisms and autoimmune diseases (table 1).
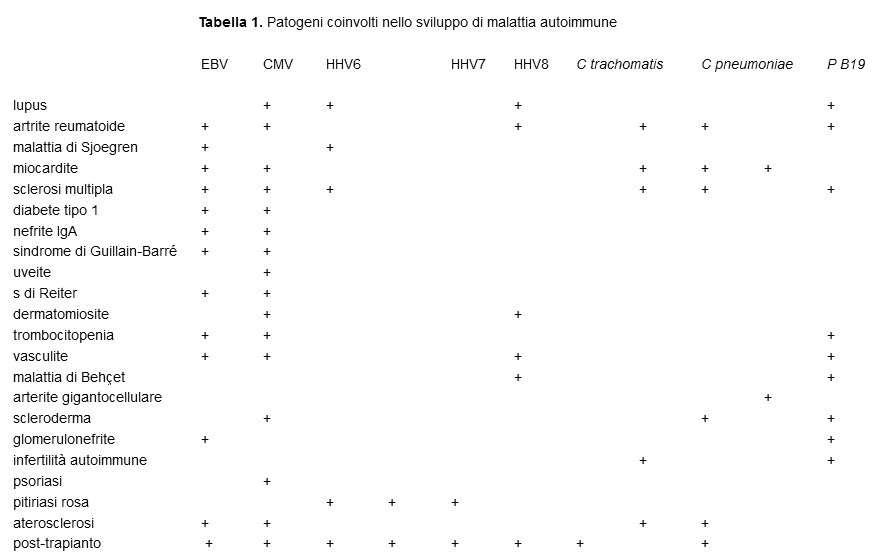
In order to develop, autoimmunity and autoimmune diseases require first of all a genetic predisposition, which must then be suppressed by an environmental factor largely consisting of microorganisms. There are numerous mechanisms through which this phenomenon develops: production of cytokines, anti-idiotype network, expression of antigens of the histocompatibility system, modifications of surface antigens or development of new antigens. However, the fundamental mechanisms are: molecular mimicry, the activation of bystander cells, the spreading of epitopes and polyclonal activation15-24.
A classic example of antigenic mimicry is the similarity of group A-hemolytic Streptococcus antigens to human antigens, which leads to the development of acute joint rheumatism when the immune system responds to the bacterium. T lymphocytes are in fact highly polyspecific, given that the T lymphocyte receptors can recognise millions of linear epitopes, but this explosive potential does not materialise as long as the common antigen is not recognised by autoreactive T lymphocytes at the same time as an infection. The activation of bystander cells occurs during inflammation and tissue destruction caused by the infection that activate the antigen-presenting cells. Epitope spreading is the next stage of bystander cell activation and triggers an autoimmune response to components initially covered by the same protein.
Conclusions
Numerous results from trustworthy research have excluded any causal link between vaccines and the development of autoimmune diseases25-28. Autoimmune diseases develop regardless of vaccinations. This is a concept that should be kept to the forefront of the mind. In addition, vaccinations never worsen the clinical course of vaccinated patients with autoimmune diseases. In conservative terms, it could be claimed that in one in every 100,000 vaccinations advances the development of autoimmunity in subjects who would have developed autoimmunity as a result of natural infection. Moreover, thanks to vaccinations 99.99% of children avoid not only infectious diseases, but also the consequent risk of autoimmune disease.
Sources / Bibliography
- Poland GA, Jacobson RM. The clinician’s guide to the anti-vaccinationists’ galaxy. Hum Immunol 2012; 73: 859-66
- Agmon-Levin N, Paz Z, Israeli E, Shoenfeld Y. Vaccines and autoimmunity. Nat Rev Rheumatol 2009; 5: 648-52
- De Martino M, Chiappini E, Galli L. Vaccines and autoimmunity. Int J Immunopathol Pharmacol (in stampa)
- Chatterjee A, O’Keefe C. Current controversies in the USA regarding vaccine safety. Exp Rev Vaccines 2010; 9: 497-502
- Münz C, Lünemann JD, Getts MT, Miller SD. Antiviral immune responses: triggers of or triggered by autoimmunity? Nat Rev Immunol 2009; 9: 246–58
- Salemi S, D’Amelio R. Could autoimmunity be induced by vaccination? Int Rev Immunol 2010;29: 247-69
- Institute of Medicine. Adverse effects of vaccines: evidence and causality. Washington, DC: The National Academics Press: 2011
- Ballotti S, de Martino M. Rotavirus infections and development of type 1 diabetes: an evasive conundrum. J Pediatr Gastroenterol Nutr 2007;45:147-56
- Hviid A, Stellfeld M, Wohlfahrt J, Melbye M. Childhood vaccination and type 1 diabetes. N Engl J Med 2004;350:1398-404
- Farez MF, Correale J. Immunizations and risk of multiple sclerosis: systematic review and meta-analysis. J Neurol 2011;258:1197–206
- Baker JP. The pertussis vaccine controversy in Great Britain, 1974-1986. Vaccine 2003; 21: 4003-10
- Coffman RL, Sher A, Seder RA. Vaccine adjuvants: putting innate immunity to work. Immunity 2010;33:492-503
- Lippi G, Targher G, Franchini M. Vaccination, squalene and anti-squalene antibodies: facts or fiction? Eur J Int Med 2010; 21:70-3
- Clements CJ. The evidence for the safety of thiomerosal in newborn and infant vaccines. Vaccine 2004;22:1854-61
- Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet 2012;379:953-64
- Eison TM, Ault BH, Jones DP. Post-streptococcal acute glomerulonephritis in children: clinical features and pathogenesis. Pediatr Nephrol 2011;26:165-80
- Kindermann I, Barth C, Mahfoud F, et al. Update on myocarditis. J Am Coll Cardiol. 2012;59:779-792
- Schessl J, Koga M, Funakoshi K, et al. Prospective study on anti-ganglioside antibodies in childhood Guillain-Barré syndrome. Arch Dis Child 2007;92:48-52
- Mayer JR, Beardsley DS. Varicella-associated thrombocytopenia: Autoantibodies against platelet surface glycoprotein V. Pediatr Res 1996;40:615–9
- Li Z, Nardi MA, Karpatkin S. Role of molecular mimicry to HIV-1 peptides in HIV-1 related immunologic thrombocytopenia. Blood 2005;106:572–6
- Yeung WC, Rawlinson WD, Craig ME. Enterovirus infection and type 1 diabetes mellitus: systematic review and meta-analysis of observational molecular studies. BMJ 2011;342:d35
- Plot L, Amital H. Infectious associations of celiac disease. Autoimmun Rev 2009;8:316-9
- Lehmann HW, Lutterbüse N, Plentz A, et al. Association of parvovirus B19 infection and Hashimoto’s thyroiditis in children. Viral Immunol 2008;21:379-83
- Chen RT, Pless R, De Stefano F. Epidemiology of autoimmune reactions induced by vaccination. J Autoimmun 2001;16:309–18
- Rioux JD, Abbas AK. The genetics of complex autoimmune diseases. Nature 2005; 435: 584-589
- Delogu LG, Deidda S, Delitala G, Manetti R. Infectious diseases and autoimmunity. J Infect Dev Ctries. 2011; 13: 679-87
- Kivity S, Agmon-Levin N, Blank M, Shoenfeld Y. Infections and autoimmunity-friends or foes? Trends Immunol 2009; 30: 409-14
- Salemi S, D’Amelio R. Are anti-infectious vaccinations safe and effective in patients with autoimmunity? Int Rev Immunol 2010;29:270-314